The Achilles Heel for Runners: Achilles Tendinopathy
Achilles Tendinopathy – the achilles heel for runners! With the nature of the last few years, many of us have had interruptions to our exercise routines. For runners especially, this can significantly increase the risk of injuries. Missing a period of training due to lockdowns or other reasons can make us want to train extra hard to make up for this gap. But this will increase your risk of injuries such as Achilles tendinopathy.
All About Your Achilles
The Achilles tendon was named after the Greek hero Achilles. This is because it was the only part of him that was vulnerable after his mother dipped him into the river Styx by holding onto his heel. That’s why weaknesses are sometimes referred to as your “Achilles heel”. Even though the Achilles tendon is the strongest and thickest tendon in the human body, it is also one of the most frequently injured.
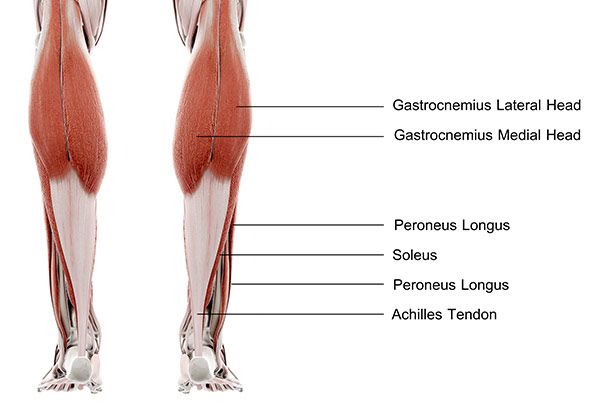
The Achilles tendon is a strong tendon that connects your calf muscle to the back of your heel. The tendon is formed from your two calf muscles – the gastrocnemius and the soleus. When your two calf muscles contract, they lift your heel up by this tendon, performing a movement called plantarflexion that is essential for walking, running and jumping.
The most common injury to the Achilles tendon is due to overuse and is referred to as Achilles tendinopathy.
What is Tendinopathy?
So what is tendinopathy? Tendinopathy is associated with characteristic changes to the tendon structure, which results in a tendon that is less capable of sustaining tensile load. It can occur in any tendon in the body, including the Achilles. You have heard tendinopathy referred to as tendinitis. This is a term that was previously used commonly to describe the changes happening in a tendon. However, this term is a bit misleading. Tendinitis implies that there is inflammation occurring at the tendon when in fact, inflammatory cells are rarely seen in biopsies of injured tendons. A better term is tendinopathy (-opathy means disease or disorder).
So if there is no inflammation, what exactly is happening to the tendon? Findings from tendon to tendon tend to vary, so there are several models that attempt to describe these changes.
One such model of describing tendinopathy is called the tendon continuum and was described by Cook & Purdam in 2008. It suggests that there are three stages to tendinopathy, as follows:
1. Reactive tendinopathy:
-
- Occurs with acute overload: e.g. dramatic increase in the number of jumping/landing repetitions, or a detrained athlete recovering from illness moderately increasing their running load. This is generally more common in younger people.
- It results in a short-term adaptive thickening of a portion of the tendon.
- This is different to normal tendon adaption to tensile load, where the tendon stiffens with little change in thickness.
2. Tendon disrepair:
-
- Similar to reactive tendinopathy, this describes an attempt at tendon healing, but with greater breakdown and increase in the number of cells, reducing overall protein production.
- This may occur across a variety of ages and loading environments.
3. Degenerative tendinopathy:
-
- This stage involves further progression and cell changes. Some areas of cell death are apparent, and there is reduced capacity to reverse these pathological changes.
- Individuals with degenerative changes often have a history of repeated bouts of tendon pain, intermittently resolving but returning as the load changes.
- If degenerative tendinopathy is extensive enough, or the tendon is placed under high load, the tendon can rupture.
Achilles Tendinopathy
Achilles tendinopathy is a common overuse injury, particularly in runners and other athletes. The incidence of Achilles tendinopathy in top-level runners is 7-9%. Achilles tendinopathy can involve a wide array of symptoms, including pain, reduced exercise tolerance, and reduction of muscle function. Pain will often begin gradually and is usually associated with increased load.
Identified risk factors for developing Achilles tendinopathy include:
- Running a distance that is too long
- Running at too high an intensity
- Increasing distance or intensity too quickly
- Performing too much uphill or downhill work
- Performing running training only without cross-training
- Poor technique
- Fatigue
Midportion vs Insertional Achilles Tendinopathy
Achilles tendinopathy can be divided into two distinct categories based on location (midportion or insertional). Treatment strategies will differ slightly depending on the location of tendinopathy.
Midportion tendinopathy is just that; tendinopathy located in the midportion of the tendon (2 to 6cm above the insertion of the Achilles tendon onto the heel bone). This is more common and occurs in 66% of cases. Insertional Achilles tendinopathy (again in the name) occurs at the insertion of the Achilles onto the heel bone (called the calcaneus).
Diagnosis
The pain associated with Achilles tendinopathy ranges from mild to severe. Typically, resisted plantar flexion is painful, and stretching your calf may also be painful. As a result, you may have difficulty standing on tiptoe or going up stairs. To begin with, you may experience pain at the beginning and end of your training, but as it worsens, you could start to feel pain throughout exercise.
You may be tender to touch along your Achilles tendon, and there could also be swelling or a thickening of the tendon. Your physiotherapist will ask you to perform some tests to check your flexibility, strength and power.
Diagnosis is often based on history and physical examination alone. Imaging may be used occasionally to confirm a diagnosis and to help plan treatment. However, the severity of findings on imaging does not always match up with the severity of pain. Abnormal findings can be seen in up to 35% of patients who have no pain at all and up to 19% of people with tendon pain with no significant findings on imaging. Therefore, in most cases, imaging is not necessary or helpful.
Treatment
Early management might include appropriate rest and activity modification. The mainstay of physiotherapy treatment for Achilles tendinopathy is to restore the tendon’s ability to withstand load. Exercises may differ based on the location of the tendinopathy (midportion or insertional).
Midportion Tendinopathy
The Alfredson protocol is the most commonly used protocol and demonstrates more significant improvements in functional measures at three months compared to the wait and see approach. The program goes over 12 weeks and consists of 3 sets of 15 repetitions, twice daily. In another trial, this program was compared to a six-week program consisting of the same exercises performed as tolerated. There was no significant difference between the two groups, but both resulted groups had reduced pain levels at the end of the six weeks. While there was no significant difference in the overall outcome, the group performing the greater number of repetitions (Alfredson protocol) reported greater pain at week three. Therefore, it may be most appropriate to use patient tolerance to determine the proper dosage of the exercise. Your physiotherapist will be able to assist you in finding the most appropriate dosage for you.
Exercises for Midportion Achilles Tendinopathy
The exercises involve performing calf raises off the edge of a step. The Alfredson program focuses on training the eccentric component of the movement – that is the part of the calf raise where the tendon is lengthening (i.e. on the way down).
- To perform the exercise, start by standing with the balls of your feet on the edge of a step and your heels hanging over the edge.
- With your knees straight, lift your heels to rise onto the balls of your feet.
- Leaving your injured side on the step, lift your other foot into the air
- Slowly lower your heel down as far as you can on the injured side
- Once you reach the bottom, put your other foot back onto the step and repeat.
- This exercise should be completed with both a straight knee and with a slightly bent knee. This ensures you work both muscles in your calf: your gastrocnemius and your soleus.
Insertional Tendinopathy
Treatment for insertional tendinopathy will be similar to midportion with one key difference. Exercises will avoid dorsiflexion (bringing your toes up to stretch the back of your ankle). The same exercises in the Alfredson protocol can be performed but on the ground, instead of on a step. This ensures the ankle will not be put into dorsiflexion.
These exercises will likely be uncomfortable for both midportion and insertional Achilles tendinopathy. Exercises should be performed to discomfort but not excessive pain.
End stage rehab will also likely include some “energy storage” tendon exercises such as jumping and hopping. These types of exercises will help the tendon regain its capacity to absorb and release energy.
Throughout and towards the end of this program, your physiotherapist will also direct you through a gradual, progressive return to your recreational activity/sport.
Recalcitrant Symptoms
For the majority of patients, Achilles tendinopathy will resolve with physiotherapy alone. However, some cases may go on to develop chronic recalcitrant symptoms. This may require consideration of additional treatments such as injections, extracorporeal shockwave therapy, or surgery. In any case, a conservative program of physiotherapy will usually be trialled in the first instance before considering additional treatments.
Recovery Time
Your Achilles tendon is slow to adapt to load, and recovery time will vary depending on the severity of the condition and your compliance with your rehabilitation program. Recovery time can vary from 6-12 weeks, to up to 12 months. Up to 90% of people with midportion tendinopathy are able to return to normal activities with little to no symptoms by 1 year.
Summary
In summary, Achilles tendinopathy is a common, degenerative, overuse condition that can be diagnosed by your physiotherapist. Treatment will differ slightly depending on the location of pain (midportion vs insertional tendinopathy) but most people will recover well with activity modification and a rehabilitation protocol that involves appropriate loading of the tendon. Your physiotherapist will be able to assist you through your recovery and get you back to performing at your best.
References
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1038.449&rep=rep1&type=pdf
https://www.britannica.com/science/Achilles-tendon
https://www.researchgate.net/profile/Tishya-Wren/publication/12092129_Mechanical_properties_of_human_Achilles_tendon/links/5ace5d414585154f3f44c430/Mechanical-properties-of-human-Achilles-tendon.pdf
https://journals.sagepub.com/doi/full/10.1177/2473011419838294
https://www.researchgate.net/profile/Tero-Jaervinen-2/publication/225039301_Achilles_tendinopathy/links/59a015d7aca27237edba41c7/Achilles-tendinopathy.pdf
https://link.springer.com/article/10.1186/1758-2555-2-30
https://clinicalphysiosolutions.com.au/wp-content/uploads/2020/08/article7.pdf
https://www.theregenerativeclinic.co.uk/wp-content/uploads/2019/12/Achilles-Tendinopathy-Longo-2018.pdf
https://journals.lww.com/acsm-csmr/Abstract/2021/06000/Achilles_Tendinopathy__Evaluation,_Rehabilitation,.9.aspx
https://www.jospt.org/doi/10.2519/jospt.2014.4720
https://www.physio-pedia.com/Achilles_Tendinopathy